Cone Beam Computed Tomography (CBCT) is a valuable tool in endodontic diagnosis. The following case illustrates how CBCT provides added diagnostic information not available through traditional 2D imaging.
This patient was referred to our office today after a long week of infection and diagnostic dilemmas. Here’s the story…
10 days ago with an ear ache.
9 days ago pt reports pain to chewing & closing teeth together.
8 days ago swelling began. Pt went to ER and was given zithromax, ibuprofen & tylenol #3.
7 days ago swelling increased under tongue and into face.
5 days ago, pt returned to ER where they did a CT scan and found nothing. Pt reports numbness in lip. Pt admitted to hospital and given IV clindamycin. MRI done and “something was found in lower left jaw”. Pt started 300mg clindamycin.
Today, patient referred from oral surgery for endodontic consult/vitality testing. Here’s how he looked.
9 days ago pt reports pain to chewing & closing teeth together.
8 days ago swelling began. Pt went to ER and was given zithromax, ibuprofen & tylenol #3.
7 days ago swelling increased under tongue and into face.
5 days ago, pt returned to ER where they did a CT scan and found nothing. Pt reports numbness in lip. Pt admitted to hospital and given IV clindamycin. MRI done and “something was found in lower left jaw”. Pt started 300mg clindamycin.
Today, patient referred from oral surgery for endodontic consult/vitality testing. Here’s how he looked.

Radiographs fairly inconclusive. #18, #19, #20, #21 all normal to percussion, probing and thermal testing.

A small crack noted on the distal marginal ridge of #18. Thermal testing once again indicates a vital pulp. Typically, we would expect a necrotic tooth to be the source of the submandibular swelling that this patient has experienced.
Since tooth #18 is responding normally to thermal testing, we decided to take a CBCT to look for more evidence of the source of infection.

This coronal slice (.25mm) shows radiolucency around the distal root #18. This image is more conclusive than the standard 2D image.
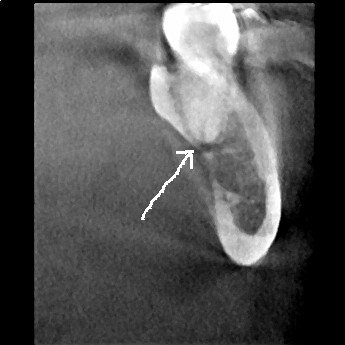
A sagittal slice through the distal root of #18 shows the lesion and its perforation of the lingual plate.

An axial view of the distal root of #18 also shows perforation to the lingual.
These CBCT slices are conclusive enough to revise the pulpal diagnosis to “partially necrotic” and recommend endodontic treatment. It appears that the distal root is necrotic and the infection is spreading through the lingual plate.

RCT initiated. Upon access, we find vital pulp tissue in the mesial canals, and necrotic pulp tissue in the distal canal.

Further removal of the distal crack finds the crack extending down the distal root, below the CEJ. Extraction is recommended.
In endodontic diagnostics, we typically classify pulpal status as:
1. Normal
2. Reversibly Inflammed
3. Irreversibly Inflammed
4. Necrotic
However, things are not always a cut an dry as that. This case illustrates that “partially necrotic” pulp is a possible classification of pulpal status.
Following removal of the tooth, the infection quickly resolved.
CBCT is an important tool for diagnostic imaging in endodontics.

